Modern life, the way so many of us work and live, has been largely devastating to the physical wellbeing of so many people. It’s implicated in record levels of chronic inflammation, pain, illness, limitation, diabetes, obesity and overweight, metabolic dysfunction, and many potentially life-threatening or limiting diseases. The medical community and a massive commercial industry often points a finger at body composition, in particular, the percentage of fat we carry, as one of, if not the main contributor to so many of these risk factors and conditions. But, what if they’re getting wildly wrong? What if there was something else, something we rarely talk about, that was the true remedy? Something that was available to all of us, and that not only held the potential to turbocharge metabolism, immunity, brain function, physical capability and mental agility, and improve mental health? And it was entirely free?
According to today’s guest, Dr. Gabrielle Lyon, a renowned physician and researcher, we’re missing something huge. She’s dedicated her career to understanding the overlooked importance of skeletal muscle for metabolism, immune function, and disease prevention. And in our conversation, she reveals how loss of muscle mass as we age, not fat accumulation, is secretly one of biggest things that undermines our health and longevity in ways we don’t even realize.
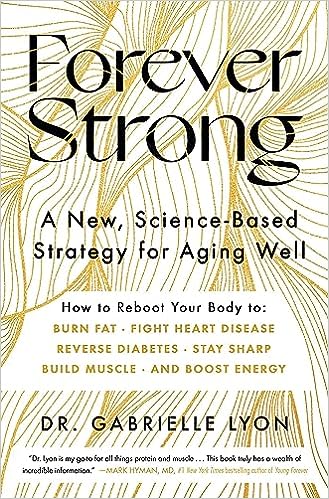
Dr. Lyon completed her medical training and a fellowship in geriatrics and nutritional sciences at Washington University in St. Louis and is a subject-matter expert and educator in the practical application of protein types and levels for health, performance, aging, and disease prevention. In her groundbreaking new book, Forever Strong: A New, Science-Based Strategy for Aging Well, Dr. Lyon shares how you can slow, stop and even reverse muscle loss through a science-based approach to nutrition and exercise.
Imagine if simply maintaining and building muscle could lower your risk for obesity, diabetes, heart disease, cancer, and cognitive decline. And just make you feel so much better and confident. Now, empowered by emerging science, Dr. Lyon is on a mission to revolutionize how we think about our bodies, movement, and nutrition as we age. If you want to thrive in your 40s, 50s and beyond, this conversation could truly change your life.
You can find Dr. Lyon at: Website | Instagram
If you LOVED this episode:
- You’ll also love the conversations we had with David A. Sinclair, Ph.D. about increasing lifespan.
Check out our offerings & partners:
- My New Book Sparked
- My New Podcast SPARKED. To submit your “moment & question” for consideration to be on the show go to sparketype.com/submit.
- Visit Our Sponsor Page For Great Resources & Discount Codes
_____________________________________________________________________________________________________
Episode Transcript:
Dr. Gabrielle Lyon (00:00:00) – Skeletal muscle is the biggest oversight. I believe in medicine today. Skeletal muscle is the organ of longevity. The health of skeletal muscle trumps the idea of body fat any day of the week. There is this beautiful interface between the health of the skeletal muscle and the action that skeletal muscle is meant to play in our life, and subsequent outcomes. All the diseases that we relate to metabolic health at its root begin in skeletal muscle first decades before.
Jonathan Fields (00:00:34) – So modern life, the way so many of us work and live, has been largely devastating to the physical well-being of so many people. It’s implicated in record levels of chronic inflammation, pain, illness limitation, diabetes, obesity and overweight, metabolic dysfunction, and many potentially life threatening or limiting diseases. And the medical community and a massive commercial industry often points a finger at body composition. In particular, the percentage of fat that we carry as one of, if not the main contributor to so many of these risk factors and conditions and focuses on treating that. But what if they’re getting it wildly wrong? What if there was something else, something we rarely talk about that was a truer, more sustainable remedy, something that was available to all of us, and that not only held the potential to turbocharge our metabolism, immunity, brain function, physical capability, and mental agility and improve mental health.
Jonathan Fields (00:01:29) – And it was entirely free. According to today’s guest, Dr. Gabrielle Lyon, a renowned physician and researcher, we are missing something huge. She’s dedicated her career to understanding the overlooked importance of skeletal muscle for metabolism, immune function, disease prevention and more. And in our conversation, she reveals how loss of muscle mass as we age, not fat accumulation, is secretly one of the biggest things that undermines our health and longevity in ways we don’t think about or realize. And Dr. Lyon completed her medical training and a fellowship in geriatrics and nutritional sciences at Washington University in Saint Louis, and is a subject matter expert and educator in the practical application of protein types and levels for health, performance, aging, and disease prevention. In her groundbreaking new book, Forever Strong A New Science Based Strategy for Aging Well, she shares how you can slow, stop, and even reverse muscle loss through a science based approach to nutrition and exercise. So imagine if simply maintaining and building muscle could lower your risk for obesity, diabetes, heart disease, cancer, and cognitive decline and just make you feel so much better and confident.
Jonathan Fields (00:02:40) – Now empowered by emerging science, Dr. Lyon is on a mission to revolutionize how we think about our bodies, movement, and nutrition as we age. So if you want to thrive into your 40s, 50s and beyond, this conversation could truly change your life. So excited to share this conversation with you! I’m Jonathan Fields and this is a good life project. So let’s dive in with sort of an opening premise of yours, which is provocative in some ways, but I think really important at this moment in time. And it’s this notion that you posit that we’re in this moment where there are a lot of things happening in our health, in our physiology, and our physical and mental wellbeing, and that the health paradigm in general has been focused in a very particular way for decades now. And you’re sort of standing up and saying, we got it wrong. So take me there.
Dr. Gabrielle Lyon (00:03:39) – Well, I think it’s important when we frame any kind of conversation where its roots lie. And I had the privilege of studying under one of the world’s leading experts in human nutrition as it relates to protein metabolism.
Dr. Gabrielle Lyon (00:03:54) – Yes, I’m a physician. Fast forward through all of that training and landing in a fellowship. I did my fellowship at Washington University in Nutritional Sciences and Geriatrics in the evenings and early mornings. I did obesity medicine research. The listener is probably thinking, well, what do all these have to have in common? Because oftentimes we think about geriatrics, which is end of life, and then we think about nutrition. And perhaps there is this interface with nutrition and obesity. And I fell in love with one of the study participants. I was working on a study that was looking at body composition and brain function, and we’ll just call her Betty. She was in her mid 50s, had three children, just an infectious nature about her. And I was absolutely taken, taken by her. And Betsy always struggled with the same £20. She was yo yo dieting her whole life. She was following the general recommendations to move more, eat less, and when I imaged her brain, her brain looked like the beginning of an Alzheimer’s brain, I felt responsible.
Dr. Gabrielle Lyon (00:05:04) – I felt that the medical community had failed her, that she had done exactly what she was told to do. And the result was that yes, had she lost weight, she’d lost hundreds of pounds over the years, regained them, and in the process destroyed her muscle. And then I started thinking, okay, well, there has to be a better solution, because it’s not that she doesn’t want to feel well or have an amazing quality of life, it’s that the information that she had been provided was not adequate. So then I started to think, seeing these patients in the nursing home at the end of life. And I don’t know if you’ve had aging parents, but we can all appreciate what that’s like. They lose muscle, they become a bit frail, even have massive memory changes. If anyone has ever known someone with dementia, it’s probably the scariest disease that anyone will ever interface with. And I started thinking, wait a second. We’ve been trying to fix this obesity epidemic for the last 50 years, and for the last 50 years we’ve gotten worse.
Dr. Gabrielle Lyon (00:06:07) – And then looking at these patients at end of life and in the Alzheimer’s units, I started to think, wait, we got this wrong, that the one thing that they had wasn’t a body fat problem, but truly it was that they were under muscle. And that’s where the concept of muscle centric medicine was born. It was a flash of insight and really a drive to change the paradigm so that we can ask the right question to get to the right solution.
Jonathan Fields (00:06:40) – So I want to dive into this a lot more. But but two things jump out at me right away. One is most physicians. And this is this is information that’s been passed to me from friends who are physicians, who have trained physicians and been med school professors, and shared that the level of nutritional training that actually is incorporated in a normal basis into medical training is incredibly small, that it’s not a huge emphasis and that it’s almost like you have to circle back on your own and really deep dive into it if you want to focus on that.
Jonathan Fields (00:07:15) – I’m curious, is that your take also? And if so, I’m curious what led you to want to circle back and say, no, this is really gonna be central to what I’m doing.
Dr. Gabrielle Lyon (00:07:23) – First of all, it is absolutely true. And nutrition science in and of itself, it’s own study. As a physician, you have to be really good at your craft to ask a physician to be really good at nutritional sciences, as well as their craft as a physician would certainly be almost like two separate careers. So that would be the first thing that I would love to lay out for individuals. For me, I came about it a bit differently. I had the privilege of moving in with my godmother when I was 17. I graduated high school early, moved in with her, and she happened to be a PhD in nutritional sciences and a trailblazer nonetheless a trailblazer in the concept. Route medicine. Really interfacing that health and wellness was rooted in what we were eating. I was fascinated, I knew at 17 that this was what I wanted to do.
Dr. Gabrielle Lyon (00:08:19) – That nutritional science is that it was a cornerstone to what made people. Well, I did my undergraduate in human nutrition, vitamin mineral metabolism, and as serendipity would have it, I landed in the class of a world leading expert in protein metabolism and was focused on muscle health from an early on perspective. The lens at which I was viewing health and wellness was different, and that never changed from there. Obviously, I went to medical school, and then I did two years of psychiatry training and three years of family medicine, and then a fellowship in nutritional sciences. So from my perspective, that’s why it’s so deeply integrated, because essentially I trained as both a nutritionist and a physician. Yeah.
Jonathan Fields (00:09:05) – Also why it gives you really unusual perspective on when you look at what ails us, when you look at the just the incredible push across every type of person in every setting and you see that commonality, it’s like you’re bringing a different lens to the experience. The other thing that I was curious about is, again, this is a conversation that I’ve had over the years with everyone from physicians to exercise physiologist to and is the notion that in medicine, often muscle is looked at in a really narrow way that, well, this isn’t this is the mechanism for mobility, and that is basically the purpose of it in your body rather than no, this is actually a profoundly important organism that affects everything else.
Dr. Gabrielle Lyon (00:09:52) – It’s the biggest oversight. I believe in medicine today. It is skeletal muscle. You’re absolutely right. Has always been thought of in its mechanical nature as making better athletes, or being stronger, or looking better, or performance. That is one small aspect of what skeletal muscle is responsible for. Skeletal muscle is the organ of longevity. It is an organ system that is responsible for so much more as it relates to our health. And in fact, the health of skeletal muscle trumps the idea of body fat any day of the week. Skeletal muscle. From a organ perspective, when you contract skeletal muscle through exercise, it secretes a molecules called myosin, which interface with the bone and the brain, and the immune system has deeply anti-inflammatory effects. Not only that, when you contract skeletal muscle, it releases glutamine, another semi essential amino acid, which glutamine is the fuel for cells of our immune system. There is this beautiful interface between the health of the skeletal muscle and the action that skeletal muscle is meant to play in our life, and subsequent outcomes to how we go through life and how we are protected, the environment that we live in.
Dr. Gabrielle Lyon (00:11:14) – And I mean, that’s not all skeletal muscle is. And I’m sure we’ll dive into aspects of this, your metabolic sink, the place where you dispose of glucose. And everybody has heard about insulin resistance and diabetes and obesity. These are diseases that are complex but are largely a muscle problem. First, obesity is not the issue. First, these challenges beginning skeletal muscle decades before there’s data from 18 year old healthy, quote, sedentary individuals with no outward signs of obesity that show skeletal muscle insulin resistance. And over time, it’s that tissue that is responsible for subsequent development of obesity, for development of insulin resistance, diabetes. It impacts cardiovascular health from the metabolic aspect. All the diseases that we relate to metabolic health at its root begin in skeletal muscle first decades before.
Jonathan Fields (00:12:16) – So let’s break this down a little bit because you’re talking about already we’re sort of like we have a couple of different things on the table. We have muscle and immune function. We have muscle and metabolic function. And not that they’re necessarily because everything plays into each other.
Jonathan Fields (00:12:30) – Right. But maybe let’s take these one at a time a little bit because I want to understand them a little bit better. So talk to me a bit about when we’re talking about muscle and metabolic function. Take me into that a little bit more.
Dr. Gabrielle Lyon (00:12:43) – Well for the women listening I’m going to make an analogy. Think about skeletal muscle like a suitcase. And let’s say you are packing for a weekend trip. Maybe you just need two days, and instead of packing for a weekend trip, you pack for 30 days in the same size suitcase. As you can imagine. What would happen is all that clothes would number one. You wouldn’t be able to close the suitcase and. Number two, all that stuff would fall right out of the suitcase. There’s no way you would be able to pack for 30 days if you are going on a weekend trip. The same can be said for skeletal muscle. Skeletal muscle is your site for 80 some percent of glucose disposal. The primary site, and number one, glucose at high levels is toxic to the body.
Dr. Gabrielle Lyon (00:13:27) – You must glucose out of the bloodstream into cells, and the primary place in which it goes is skeletal muscle. Number one, it is stored as glycogen. And I think that we’ve all heard that from an athletic perspective. Glycogen is the storage form of carbohydrate in skeletal muscle, but that only allows for a certain amount of storage if you are not exercising. Once that muscle is full, there is nowhere else for blood glucose to go. So we see a rise in in glucose in the bloodstream and a subsequent increase in insulin, and also an increase in things like fatty acids back into the bloodstream. This becomes a challenge because these all over time generate metabolic dysfunction. The health of the skeletal muscle declines. Another way to think about this is a filet. You want your skeletal muscle to look like a filet. If you’re not exercising over time, that muscle will look like a ribeye steak. And that is a very simple way that the listener can really think about what and how does the quality of our tissue change if it remains untrained?
Jonathan Fields (00:14:38) – When you think about metabolic function, there’s this term that’s been batted around over a period of years.
Jonathan Fields (00:14:43) – I don’t know if it’s still I haven’t heard it as much recently. Metabolic syndrome. This was a whole bunch of different quote symptoms were folded into the syndrome. I guess syndrome is when it’s not necessarily identifiable disease. But you sort of you look at all the symptoms and say, okay, this thing is going on. Is this part of what you’re talking about? Here it.
Dr. Gabrielle Lyon (00:15:00) – Is. And you’re absolutely right. People don’t talk a lot about metabolic syndrome, but this skeletal muscle is a primary site for metabolic syndrome, which will see elevated levels of blood sugar, elevated levels of triglycerides. You may even see elevated levels of hypertension. So you might become hypertensive. Yes. And I also want to frame this in the way that when you have heard individuals talk about metabolic syndrome, it has all been based around obesity. It is all been based around body fat, never about root cause and quite frankly, root cause as something that we can do something about. You know, again, this book for ever strong.
Dr. Gabrielle Lyon (00:15:40) – The goal of it is to really shift the perspective from this idea that we always have something to lose. It’s always about weight loss. It’s always about fat loss, too. What do we actually have to gain? What do we have to gain? And what we have to gain is skeletal muscle. This becomes very empowering and a very empowering conversation, especially for women, especially for anybody who is aging, because there are time periods in our life where we are vulnerable and as we age, the vulnerable places like menopause or for men, when we see a significant decline in testosterone. These are the times where the body is most vulnerable to skeletal muscle loss. And it doesn’t have to be that way. But if we continue to eat and think about the weight loss perspective that we’ve had potentially in our 20s and we carry through those habits, ultimately we’ll destroy our tissue. And we’ve seen that. We’ve seen that with sarcopenia adults, which is a loss of muscle mass and function. And quite frankly, we’ve seen it with, you know, our parents, our grandparents, when they become skinnier and more frail.
Dr. Gabrielle Lyon (00:16:53) – These are all diseases of skeletal muscle. And most importantly, it’s never too late. So with particular strategies that can be leveraged, these challenges that we see later on in life that are related to skeletal muscle mass can be addressed. Decades earlier.
Jonathan Fields (00:17:10) – You brought up the notion of what happens to muscle over time as we age. Also, and actually I want to dip into that. But before we get there, I also want to address, you know, we talked about the importance of muscle and metabolic health, but you also you hinted at the notion of our muscles being critically important in our immune function, in our risk for various different types of diseases or lack of risk or reduction of risk. And I think that’s probably a less intuitive leap for a lot of people.
Dr. Gabrielle Lyon (00:17:41) – It is. And that’s actually why I brought it up, because we can all agree that skeletal muscle is important for mobility and being able to take care of activities of daily life. We can all agree upon that. And I think the notion that skeletal muscle is a focal point in metabolism is also pretty intuitive, right? We know that the more healthy muscle mass we have, then we have places to put substrates or foods that we eat less.
Dr. Gabrielle Lyon (00:18:06) – Thought about is skeletal muscle as an endocrine organ. What does that mean? That means contracting skeletal muscle releases. Myo means myo kinds are hormones that travel throughout the body. They act locally, but they also act on nearly every tissue, these myo kinds. And I’ll just name one or I’ll name a few. But the most famous is interleukin six. And for the savvy listener, they’re probably thinking, well, wait a second. Interleukin six is a cytokine. And we’ve all heard about cytokine storm. And interleukin is a a cytokine that’s released from macrophages. And it really creates a ton of systemic inflammation. Well. When interleukin six is released from skeletal muscle contracting skeletal muscle, it actually helps interface with interleukin six and interleukin 15 released from other parts of the body to actually help dampen that immune response. Where does this play out? Let’s say you are not in a major cytokine storm, or you don’t have a ton of active inflammation from an acute issue. Let’s think about how this plays out from, say, for example, a rheumatic disease or a disease that are affecting the joints or autoimmune conditions.
Dr. Gabrielle Lyon (00:19:24) – Exercising skeletal muscle can help interface with that inflammation to lower it and allow the body to respond in a more, for lack of a better term appropriate way. And that that in and of itself is fascinating. What also is fascinating is that the amount of kinds you release, or interleukin six, is directly related to the amount of exercise that you’re doing. Incredible. And this is some of the earlier work from Pettersen. She’s now in Copenhagen. She’s an immunologist and also a physician, and her work is really paved the way to begin. It hasn’t really hit so much in the US, but has begun to pave the way again. Research takes a decade to interface with the general population. If not, I think that the average they say is like 17 years. But this information is out there. And once we recognize that exercise, which, by the way, 50% of Americans don’t do that once we can prioritize skeletal muscle. And if I can influence the listener to believe that it is so critical and that the amount of effort that we put into our training will have subsequent effects, not about body composition.
Dr. Gabrielle Lyon (00:20:36) – Like, let’s put that on the back burner, but how it relates to immune function. And that’s just one area. People really care about cognition as they age. Exercise using skeletal muscle can release something called sepsis and B and Iverson, both which stimulate Bdnf, which is brain derived neurotrophic factor that influences neurogenesis, the neurons in the brain to be healthy. And this is again, so critical when we think about how we want our life to be. And then I’m going to also throw something else out there that I think is really important. And it’s a little esoteric, but the idea that skeletal muscle is this currency. And when we think about currency, we think about things that we can buy or sell or bargain for. But skeletal muscle is your health currency, but it’s the most unique health currency in that the action that you have to take to gain it influences the person that you must become when you begin to execute these actions with discipline. And that’s something that I believe is a little bit overlooked because there is this sense of empowerment.
Dr. Gabrielle Lyon (00:21:42) – I’ve never had someone come to me and say, you know what? I really regret being strong. I really regret who that made me. I really regret the discipline it took to prioritize in my schedule an action and then subsequent feeding plan or nutrition plan that became a lifestyle. So I know that that doesn’t directly relate to the immune system. But people are global. We are global individuals and we have to have global strengths. And global strengths are not just muscle and body composition. There is a mental fortitude and a grittiness that an individual develops when they develop this currency.
Jonathan Fields (00:22:16) – Yeah. I mean, couldn’t you actually make the argument that it does relate to the immune system in that we know that state of mind actually has a direct impact on the state of immunity. So if exercising increases lean body mass increases muscle. And that makes you feel stronger, more confident, more able, and that makes you feel just more connected to yourself and more capable of being in the world that we want to be. That that would affect your mindset in a way that would potentially then create this positive cascade back into the immune system and help boost it.
Dr. Gabrielle Lyon (00:22:49) – I couldn’t agree with you more. I didn’t want to go too far out on a limb and lose the listener because it’s okay, I’ll go there. I really want them to leave this conversation with a sense of empowerment, because if we can shift the paradigm of thinking around skeletal muscle and it’s not just some Brody thing, but that it really is the focal point of disease prevention and just longevity and aging, then we can really change the conversation. And that’s actually why I named my book Forever Strong. And it’s not just strength. It is, again, global strength, mental and physical and emotional strength, which, by the way, I think about as a physician, I know you’ve had many physicians on the show and spoken to many physicians. They will all tell you that a good physician recognizes patterns of diseases and patterns of illness. That is, the craft of a physician, the art of medicine, the true art of. Medicine is recognizing patterns of people and what obstacles lay in front of them from taking action.
Dr. Gabrielle Lyon (00:23:53) – And I talk all about that in the book, too, because I could provide you with a perfect plan. But unless you are aware that there are certain things that may be underlying that stop you from taking action like a self worthiness temperature, understanding that you have to feel worthy of getting the body that you want of being and having the health that you feel that you deserve, all of that has to be addressed.
Jonathan Fields (00:24:19) – Yeah, that makes so much sense. So if we, in the context of the role of muscle in immune function and hopefully avoiding disease risk, illness risk, if we drill it down to just take one common thing. So by the time many folks have reached the mid years of their lives, many an alarmingly high number of people have been diagnosed with some form of what would be labeled autoimmune disease dysfunction. So I think people walking around with autoimmune conditions has become such a common experience. Probably so many people who are listening to this conversation right now have either dealt with it or are dealing with it right now.
Jonathan Fields (00:25:01) – So if we just sort of like look at that as an example and say, well, how would potentially exercise and improving our muscle mass in our body affect an autoimmune condition? Walk me through that.
Dr. Gabrielle Lyon (00:25:15) – Well, obviously autoimmune conditions are pretty complex. And I’ll walk you through one of the most common. Let’s talk about Hashimoto’s. Hashimoto’s is a very common autoimmune condition that attacks the thyroid, and an individual’s thyroid is being attacked by their own cells. How would exercise play a role in this? Well, again, Hashimoto’s is complex. There’s genetic, there’s environmental influence. There’s a whole host of things that happen when we think about skeletal muscle. We have to think that one of the the focal points of thyroid of hypothyroidism is this autoimmune attack low levels to moderate levels of systemic inflammation over time. You could you just treat Hashimoto’s with skeletal muscle? No, I would say that you couldn’t. But one thing is for certain the more unhealthy skeletal muscle mass you have, the more you are going to suffer from the consequences, like obesity or insulin resistance or elevated levels of blood sugar.
Dr. Gabrielle Lyon (00:26:18) – This all will make thyroid and other autoimmune conditions more difficult to treat, because it will continue and perpetuate this autoimmunity. Again, I’m saying this in in kind of global terms, because there’s other things with Hashimoto’s, like understanding what the trigger is. Are there issues with gastrointestinal health? I mean, we see a lot of individuals that suffer from Hashimoto’s thyroiditis that have gut infections. But the other aspect of this is it can become a vicious cycle. Oftentimes, many of these patients are hyperthyroid with hyperthyroid. One of the first indications is either fatigue or a massive gain in weight. This is all impacted in skeletal muscle. You require a healthy level of thyroid hormone to influence the use of glucose getting into the cells of skeletal muscle. But that’s all at rest. When you have exercise, you no longer require insulin. You are able to address moving glucose out of the bloodstream into tissue without the use of insulin, and that becomes important because, again, with hypothyroidism, one of the aspects of metabolism that are affected or that is affected is these glute four receptors, which we don’t necessarily have to go into detail about that, but it’s the capacity of muscle to utilize glucose can decrease.
Dr. Gabrielle Lyon (00:27:41) – And so that’s just one aspect of how having healthy skeletal muscle and also exercise can help with an autoimmune condition.
Jonathan Fields (00:27:51) – And that makes sense when you sort of trace the pathways. The other thing that I’m curious about is cancer does good exercise and and muscle volume or muscle mass on your body. Can that actually have an effect on something as pernicious as cancer? And again, cancer is is an umbrella term. There are so many different types and forms and approaches. But on something like that can it actually have an impact?
Dr. Gabrielle Lyon (00:28:13) – I appreciate, Jonathan, what you’re saying. Cancer is highly complex. You could do everything perfect and still get it. So we’re certainly not saying that. But there is one major risk. And of course we have to define what kind of cancer are we talking about. Are we talking about colon. Are we talking about breast. There is one unifying major risk factor of cancer as a whole. Do you know what that is? Obesity. How do we combat obesity. Where does obesity start? Skeletal muscle.
Dr. Gabrielle Lyon (00:28:41) – Having a good and solid body composition with healthy skeletal muscle can greatly improve your percent body fat, right? Assuming that you are exercising doing these things. Because we know that being obese or having obesity is a risk factor for cancer, and then that’s not even talking about the interface with inflammation. Again, we spoke about contracting skeletal muscle interfacing with cells of the immune system. And it has a whole host a whole plethora of other effects. But cancer is also a big one. And I also highlight this in my book exercising skeletal muscle having healthy skeletal muscle. Protecting metabolism access by. It can really disrupt estrogen production. It can increase the amount of estrogen an individual produces over time. That’s not a good thing, right? You don’t want excess levels of estrogens that are driven through adiposity. Other things with excess body fat that we see are elevated levels of HCP, which is an inflammatory protein produced in the liver. This is a risk factor for cardiovascular disease. Once we begin and go down that road, there’s also increased levels of triglycerides, endothelial dysfunction, Othello sclerosis, which we’ve all heard about.
Dr. Gabrielle Lyon (00:29:58) – Again, it’s not that things are independent. They are all interdependent. And we have to pull the lever of the thing that we can do something about. And the thing that we can do something about clearly is skeletal muscle. Whether you are putting on skeletal muscle when you are exercising and you are prioritizing resistance training and strength training, you get stronger.
Jonathan Fields (00:30:20) – I want to tease out a distinction here also, because we keep referencing a number of times you’ve referenced the relationship between skeletal muscle or body composition. And so our body is made up of different types of tissue, lean tissue, fat tissue. When we think about how does having more muscle potentially reduce body fat. And again, we’re not talking about cosmetics here. We’re talking about health. I think it’s intuitive that a lot of people think, well, like if I have strong muscles I can exercise more, which means like we’ve all learned in high school bio, I’ll burn more calories. And, you know, but I don’t want to miss another part of this, which I’d love you to walk me through a little bit, because maybe this is less intuitive.
Jonathan Fields (00:31:02) – My understanding is that muscle is actually the most metabolically active tissue in the body, even at rest. So it’s part of what we’re talking about, the notion that simply having more of this tissue on us, whether we’re exercising or not, even when we’re sleeping, will make us more metabolically active. And even without us actually contracting that muscle have an impact, potentially on body fat and on inflammation, on all these other things.
Dr. Gabrielle Lyon (00:31:30) – I think a great way to think about it is skeletal muscle makes up 40% of body weight. And so based on mass, the amount of mass you have is really what influences the metabolism. Where the magic of muscle happens is really through that contraction. That’s where you can bump up the amount of calories that you’re utilizing. Again, muscle mass and all lean tissue. So brain is actually incredibly dynamic. It might use up to 27% of just our basal metabolic rate for that small organ. So based on mass is skeletal muscle highly active. The magic of the mass I think really comes from the exercise.
Dr. Gabrielle Lyon (00:32:13) – Again, the exercise component where the other influence of tissue comes from is. So when we think about overall how many calories we burn, how many calories we burn at rest, there’s, you know, total daily energy expenditure. And then there’s a portion of total daily energy expenditure that comes from all lean tissues and that supports bone turnover, liver, brain, etcetera, all of the tissues and skeletal muscle, again based on mass houses, because it’s 40% does contribute a considerable amount to that total energy expenditure. So I do think that that is important. And then the important distinction is really what you do with that mass. But there’s something else that’s really important that you bring up because of its mass. It also houses an enormous amount of mitochondria. And mitochondria can be metabolically active even at rest. And this is the site for energy production, ATP production, fatty acid oxidation, and quite frankly, skeletal muscle at rest burns fatty acids. When you think about having healthy skeletal muscle, there on, you can think about having a better cholesterol profile.
Dr. Gabrielle Lyon (00:33:29) – Think about it from that standpoint. There’s 40 million people on statins. Do we all need to be on statins, or do we need to leverage the fact that at rest skeletal muscle burns fatty acids?
Jonathan Fields (00:33:43) – Are you aware of research that looks at body composition and versus lipid profile?
Dr. Gabrielle Lyon (00:33:50) – Oh, I’m going to say yes, certainly. And then I’m going to say we haven’t been directly measuring skeletal muscle mass by the way. Which is again, what does this point to this point to the large oversight of the importance of skeletal muscle? Is it because technology wise, they haven’t been able to do it? I think it’s more just the oversight of the importance. And once we put a paradigm in place, we just continue to talk about that paradigm. For example, Dexa, I don’t want to go down a rabbit hole unless you ask me to, but everybody looks at Dexa, which actually Dexa measures. Bone and fat, and the rest is extrapolated, and that includes all lean tissue. And when we talk about lean body mass, you know, 40% of that is skeletal muscle.
Dr. Gabrielle Lyon (00:34:31) – But what about the other 60%? It’s other stuff. So I think that that’s a real important distinction. But your original question is, do you see improvements in a lipid profile with lower body fat and higher skeletal muscle mass? Yes, you do. And in fact, in some of the earlier studies out of Don Lehman’s lab, and I worked on some of these earlier studies, we looked at two groups of individuals. Again, he’s worked on a lot as an undergraduate. You never get your name on the paper. It’s just part of how it goes. And over the years he’s done multiple different studies. One study looked at two groups of individuals. One group had their dietary profile was around the food guide pyramid. So 51% carbohydrates. And then it was, I think around 10% protein. The other group was more of a zone diet. It was a 40% carbohydrates, 30% protein, 30% fat. Both groups struggled with obesity. What they found was that when you corrected for dietary protein, and you added in a very small amount of resistance training, two days a week of yoga.
Dr. Gabrielle Lyon (00:35:34) – And by the way, they looked at triglyceride levels. They looked at blood pressure, they looked at all the metabolic syndrome picture. Those individuals improved skeletal muscle mass and lost a significant amount of body fat. Their blood lipids improved, their blood sugar improved versus the other group that was still calorie restricted. Again, that’s the story of Betsy over and over and over again was still calorie restricted, but they lost 35% more lean tissue, which was both muscle and whether it was bone or liver or any of these other organs. And their blood sugar actually went up, insulin went up and triglycerides went up.
Jonathan Fields (00:36:18) – Yeah. I mean, it’s kind of alarming.
Dr. Gabrielle Lyon (00:36:19) – It’s alarming because we have to be able to give and provide good information and appropriate information. We’ve done the model of eat the food guide pyramid and exercise more, and we see that in the data. Those individuals really lose lean tissue if they are not exercising.
Jonathan Fields (00:36:36) – It really also reinforces the notion that regardless of what reason, somebody may feel like, oh, I need to go, quote, lose weight.
Jonathan Fields (00:36:44) – That’s so often the approach that is attached to that doesn’t consider. But what are the where am I losing weight from, you know, because you’re not just saying, well, I’m going to lose £20, that’ll be £20 of fat. That’s what I determine. It’s like, no, you’re actually you’re taking away some of this really critical metabolic tissue when you’re doing that, unless you’re actively doing something to counter it along the way. And also really understanding that how you eat while you’re doing that makes a difference in how you move and all these different things along the way.
Dr. Gabrielle Lyon (00:37:15) – And, Jonathan, I’m going to point out something great that the good news is the good news is 100% of people eat. And you can definitely move the needle by doing the thing that most people do every day. That’s amazing. Getting that nutrition piece right from an evidence based perspective is mission critical. And then on the flip side of that, it doesn’t take much exercise to maintain the health of that tissue, to maintain the health of skeletal muscle and protect that tissue as you’re going through periods of weight loss, very minimal.
Dr. Gabrielle Lyon (00:37:47) – Again, in some of the earlier studies, you’re talking about two days a week of walking in yoga.
Jonathan Fields (00:37:52) – Yeah. Which most people can fit in. Let’s talk about those two different interventions a bit more than nutrition and movement. And let’s start out with nutrition. So often we start by looking at these or conventional government dietary guidelines and traditional things that we’ve been told to try and help figure out. And that was taught, you know, that was taught in schools, that was taught that was sort of like the, you know, what the Ada was putting out there and say. And from your perspective, what are the guidelines get wrong that we need to address?
Dr. Gabrielle Lyon (00:38:26) – First, we have to think about where the guidelines came from and why they’re here. Guidelines are not necessarily for optimizing health. They’re really to prevent deficiencies. And when we think about the history of the guidelines, these dietary guidelines were born on the heels of the Great Depression entering World War Two when they drafted the first million soldiers and they found 38% of them were either flabby or had malnutrition.
Dr. Gabrielle Lyon (00:38:56) – When the country was faced with losing everything, a way of putting it declared an emergency, a nutrition emergency they didn’t mean wasn’t there. So I don’t know if they declared a nutrition emergency, but they pretty swiftly got a committee together, and they realized that in order for us to protect our country, that we needed strong, capable individuals. So this was in the early 1940s. In the early 1940s, they recognized that dietary protein was critical. And again, getting to these recommendations, they recognized the dietary protein was critical. They didn’t. Nutritional scientists was still very new and arguably is still very new. But they made some certain recommendations. And what they said was in order to help Uncle Sam, you needed to have high quality proteins. So they recommended liver and beef and eggs, etcetera, for muscle health because they wanted vitality and they wanted strong humans, which, when you think about it, that was profoundly insightful in the 40s. The other pamphlet that they released was if you wanted to help Hitler, what would you do? You would eat highly processed foods.
Dr. Gabrielle Lyon (00:40:09) – You would just eat white breads. You would limit all your protein. You would again eat this highly processed, low protein diet. The guidelines then ultimately came up with this information that based on nitrogen balance studies, which to my knowledge and to anyone’s knowledge, nitrogen is not a outcome that we look at for health. They determined that the recommendation for preventing deficiencies was 0.8g/kg, and that was equivalent to 0.37g per pound ideal body weight, and.
Jonathan Fields (00:40:45) – That would be of protein of.
Dr. Gabrielle Lyon (00:40:47) – Protein for a £115 woman, that recommendation is around 45g of protein, 115 times 0.37 is about 45g of protein. Those recommendations so fast forward from 1943 to 1968, when they really made those recommendations, they had to think globally. What is a global recommendation that we could make that would prevent deficiencies? Because the RDA is not just us, it’s not just the US influence. It’s again sustainability for the entire world. Right? So the US can’t be recommending a diet that is triple the amount of protein versus India or China. How are they also going to be able to meet that need.
Dr. Gabrielle Lyon (00:41:34) – But that recommendation for dietary protein again was based on the minimum to prevent deficiencies based on nitrogen balance studies. Nitrogen balance is just an old school way of looking at the amount of protein needed to maintain tissues, etcetera, and to not become to a deficient state. Those recommendations have not been changed since 1968, which means one of two things do we not have any new science, or are there other influences at play that have overshadowed the need to readdress dietary protein? Fast forward to decades of literature. It shows in the literature that double the RDA is much more optimal for healthy aging, but yet to even be addressed. It has not been addressed yet. There is mounds and mounds of evidence.
Jonathan Fields (00:42:24) – So is this political or commercial?
Dr. Gabrielle Lyon (00:42:28) – When we have a conversation about nutrition nowadays, I think that it’s very rarely about solely empiric data. The conversations and the landscape around nutrition and health are typically cloaked in morality, agenda, personal belief, childhood thoughts, whatever it is. But we solely are not talking about the empiric data of what is shown to be more optimal for humans.
Dr. Gabrielle Lyon (00:42:53) – Yes. Do I think it’s political? For sure. We could probably all agree that. Or is a very political conversation around nutrition. And that, my friends, is exactly why I wrote the book. That is one reason why I wrote the book, because I also highlighted some of this history. If we do not understand the lens at which we view things, then we become blinded to the information that comes out there and to the origin of the information. I’d love to just highlight something. Give you an example of what that is. Yeah, sure. In the 40s, the early 40s, the government recognized how important Whole Foods were, how important whole proteins were, butter, milk, etcetera, how important fruits and vegetables were. A commodity is a whole food. A whole food commodity would be something like beef or pork or corn or soy. They are unprocessed, whole foods from farmers collectively, the commodity which is under the jurisdiction of the USDA. Collectively, they pool their resources together to have a marketing budget.
Dr. Gabrielle Lyon (00:43:59) – That means all the farmers, they go into a checkoff, all the dairy farmers, all the beef farmers, all the corn producers, etcetera. You don’t hear about individual almond farms or individual milk farms, right? When you see an ad for almonds, it’s almonds, right? California’s almonds. Or when you see an ad for milk, it’s milk. Does a body good. When you see a beef, it’s beef is what’s for dinner. You don’t see individual farmers. Commodities. Collectively, their marketing budget is $750 million for everybody. They also, under the USDA, cannot say anything disparaging against any other food. So the commodities could not say, well, you know what? A real burger is better for you than a fake meat burger. A real burger has more bioavailable protein than X, Y, and Z versus the processed food companies. And we’ll just pick one. We’ll pick PepsiCo. That one company alone, its marketing budget is almost $2 billion. For one company, you can imagine who controls the the money can control the narrative.
Dr. Gabrielle Lyon (00:45:10) – Any processed food can say something disparaging against another food source. A fake plant based milk could say it’s better for you than milk is a fake processed burger could say it’s better for you and the environment than a beef burger. Just because it is said, doesn’t mean it’s true. And that becomes really important. And that is a place of great confusion for the consumer. The lens at which they are receiving information, the balance is off. It is not an equal opportunity information exchange.
Jonathan Fields (00:45:45) – Yeah. And at the end of the day, it makes you wonder why the typical person has a bit of a, you know, the head spins when they’re trying to figure out, I know what’s the truth when it comes to what I should put into my body. And, you know, because it’s the information is coming from so many different sources and there are different limitations or opportunities at different sources have also and it all comes at us and we’re left to sort of say, well, what do we do with the fire hose of information? And it seems like so much of it just keeps conflicting each other.
Jonathan Fields (00:46:18) – It’s almost like the average person, the average human being, is a bit left to fend to themselves to really try and suss out, like, what is the truth here? Like, what should I really be doing and thinking about? I mean, just then the basic notion going back to the early part of the conversation about protein, like the fact that it’s been almost 60 years and there’s a lot of empirical data, a lot of science that’s come out in those six decades or so that hasn’t been really actively folded in just around this one substrate, just around the idea of protein and how actually, like we may need substantially more, especially as we age.
Dr. Gabrielle Lyon (00:46:53) – We absolutely need more. And what is so crazy is that when you think about macronutrients, we think about fats, carbohydrates and proteins. And unfortunately it is like the black sheep of the macronutrient family. There is so many heated discussions around dietary protein. When anything becomes that emotional, it really clouds the judgment and also the information. And again, you have to remember, I’m a trained geriatrician.
Dr. Gabrielle Lyon (00:47:21) – I am trained to take care of people who are aging. And within that window of opportunity, getting dietary protein and exercise correct is going to create a life and at least something that you can choose so that you can protect yourself and your family and the people that you love. And again, my book, Forever Strong, it is an evidence based book. And it is it is to clear up this narrative, to empower people so they are not distracted by the chaos making machine, because the window of opportunity will close, and having really good, solid information so that an individual can execute is again, mission critical. Right now it’s mission critical.
Jonathan Fields (00:48:07) – And the window closing part of the process, as you describe as we age, if we don’t do something to actively counter the loss of muscle in our body, it starts to effectively shed. Every decade we have less and less and less of it and less. We are proactively saying, I’m going to do something to to counter that process. Part of it is adjusting what we take into our body like the protein intake.
Jonathan Fields (00:48:30) – The other part that I want to get to is, and we’ve kind of reference it loosely, is exercise because this is not just about mobility and about burning calories and about lowering inflammation, but but the amount of muscle that we have, if our body is naturally shedding muscle, if we don’t do anything to counter in the process is less and less every year. Once we hit sort of the middle years of our lives and we know exercise is really critical, how much can we actually stop that process versus just saying, like, let me just save what I have versus actively continue to build or add muscle tissue to our body? And is there a point at which it becomes harder and harder to actually add or even sustain?
Dr. Gabrielle Lyon (00:49:14) – First off, you can always get stronger and you can always add muscle mass. Again, if you are an athlete and you’ve hit some genetic potential, perhaps it becomes much more challenging. But again, you should always be able to improve in. Some metric and for the listener. Wherever you are starting, it’s a perfect place to start.
Dr. Gabrielle Lyon (00:49:35) – It is more challenging to build muscle as you age for a few reasons. I say it’s more challenging. Can it absolutely be done? Yes. Has it been demonstrated to be done? Yes. I still see patients. I have a clinic. I still see patients. We see older individuals building skeletal muscle to this day. Age is not a limitation. By highlighting some of the changes that skeletal muscle goes through, we can implement strategies that are answers to those changes. I mentioned earlier that skeletal muscle is a nutrient sensing organ. If I didn’t, then I should have. And it senses the quality of the diet. In particular, it senses the branch chain amino acids, particularly leucine. I will take a moment and step back and say, when you hear about protein, you hear about it as if it’s one generic term, but frankly, it’s 20 different individual amino acids, all of which should be thought of as individual nutrients. Therefore, protein sources are not interchangeable. They all have different profiles of these different amino acids.
Dr. Gabrielle Lyon (00:50:44) – When it comes to skeletal muscle health, leucine is critical. Leucine for an aging individual. How do you get leucine in the diet? Leucine is typically found in high amounts in high quality proteins. High quality proteins are by definition based on an amino acid profile, meaning they have high amounts of the essential amino acids. These are amino acids that we must get from the diet, and high quality proteins are things like whey protein, beef, eggs, fish, typically animal based sources. Lower quality proteins, by definition, have lower levels of those essential amino acids. What becomes important to highlight here is that as we age, it is very important to hit something called a leucine threshold. And this came out of this early work came out of John Lehman’s lab, who trained me, where he really put the connection between leucine dietary protein and this mTOR signaling and muscle protein synthesis. So it’s essentially putting the key into the car and turning on the car when you hit a leucine threshold, and that would be in 30g minimum of dietary protein could be a scoop and a half of whey protein.
Dr. Gabrielle Lyon (00:52:02) – It could be some Greek yogurt. It could be a small four ounce chicken breast or steak, something like that. Obviously it can be a combination of different foods, but when you hit that high quality protein and that leucine threshold, it triggers something in the muscle, and it triggers this physiological process called muscle protein synthesis. Muscle protein synthesis simply is this incorporation of amino acids into tissue. This process becomes less efficient as we age. It’s called anabolic resistance. Anabolic resistance can be overcome, and older tissue can respond like younger tissue by increasing the amount of protein at one meal. And the evidence supports that. We know that when you are subthreshold over time, let’s say you wake up in the morning and you have 20g of protein, you’re not hitting that threshold. And over time, that will affect this maintenance of lean tissue and maintenance of skeletal muscle. I know that we wanted to talk about exercise, which we will, but from a physiological perspective, it’s important to understand what’s happening in skeletal muscle. There is a synergistic effect of adding in exercise with dietary protein.
Dr. Gabrielle Lyon (00:53:23) – When you train, do resistance training and add in high quality protein. Let’s say it’s 20g of protein. There is a synergistic effect that happens within skeletal muscle, older skeletal muscle, which is kind of what we’re getting at it and thinking about. Part of the reason is more blood flow. We’re now bringing blood flow. We’ve now sensitized the muscle. The muscle is ready to receive nutrients. And that is a very simple way that everybody can take action. That first meal of the day is most important hitting if you are older, between 40 and 50g of dietary protein. I know that sounds like a lot. You can do it through a shake again. You can do it through some Greek yogurt. There’s multiple ways to do that, but that’s really important. And if you say to me, well, Gabrielle and Jonathan, that’s way too much. I would say do your resistance training and then give me 30g of dietary protein and you protect tissue.
Jonathan Fields (00:54:17) – As you’re saying this, I’m just saying to myself, I’m not usually hungry in the morning, so I don’t eat breakfast.
Jonathan Fields (00:54:22) – And I’m like, hmm, I might need to start rethinking things a little bit.
Dr. Gabrielle Lyon (00:54:25) – You can train yourself. And the reason a lot of people are not hungry. I’m particularly not hungry in the morning, and that’s done and served individuals who do intermittent fasting very well. My suggestion would be to push that feeding window earlier. So, Jonathan, if you are more mature in age then having a protein breakfast again, maybe it’s a 10:00. I’m okay with that. But making sure that you’re not then in a catabolic state an overnight fast would be a catabolic state. How long are you willing to go? If you did resistance training in the morning, then that would stimulate skeletal muscle. But the body is turning over easily 250g of protein a day. You’re not eating 250g of protein a day. Your body must be able to meet that need. As you continue to be in a catabolic state, the body will pull from amino acids in skeletal muscle. We don’t want that.
Jonathan Fields (00:55:19) – Yeah, no, that makes so much sense.
Dr. Gabrielle Lyon (00:55:21) – I don’t recommend long periods of fasting, especially if you are more mature. That is a nice way of saying it.
Jonathan Fields (00:55:27) – Right. Which is also interesting because intermittent fasting, this sort of like the 16 eight window has become so in vogue these days, and often it’s for those people who implement it. It’s sort of like a fast which goes the feeding window is noon to eight. So maybe if we’re a little further into life, it makes sense to really rethink that. Even if you want to have a commitment to some form of intermittent fasting, to maybe shift the time window a bit and also really think about the macronutrient breakdown. And also when you’re moving exercise into that. When you mentioned resistance training, and I think everyone was probably heard, like the best way to build muscle is resistance training. Is that still the state of best information?
Dr. Gabrielle Lyon (00:56:09) – I would say that it is a non-negotiable and resistance exercise can make take many forms. Originally I would think you would have to lift heavy. That was always my thought process.
Dr. Gabrielle Lyon (00:56:19) – It doesn’t have to be that way. We have to recognize that lifting heavy may stimulate some processes that are different than lifting light, but both what we’re ultimately going for is for an adaptation, and that is why we are doing resistance training. There’s multiple ways to do resistance training. We do know that it is just for definition. It’s a you’re moving something against force, and that force could be your own body weight. That force could be a band, it could be another kettlebell or dumbbell, you name it. But that’s what the goal of resistance training is. It’s how it is defined. And again, we are looking for adaptations, whether we are looking for muscle strength and size or muscular endurance, do you have to lift heavy weights to do some of these things? You don’t, but the act of resistance training versus cardiovascular activity, I think this is the non-negotiable for exercise and body composition. This is the non-negotiable for maintaining the skeletal muscle that you have. And again, can you get away with lower loads.
Dr. Gabrielle Lyon (00:57:21) – So could you do a rep range that is above 12 reps? Totally. I basically start individuals at three days a week, ten sets per muscle group, however you want to fit that in.
Jonathan Fields (00:57:33) – You also mentioned which my eyebrow raised a little bit earlier in one of those initial studies that the twice a week training one of the exercises was yoga, and I would imagine a lot of people would look at that and say, well, does that actually count as resistance training?
Dr. Gabrielle Lyon (00:57:49) – It does in the beginning. Again, we’ll work towards progressive overload, but you are moving against a force. It is somewhat of a form of obviously stretch and, and these things. And there is, is that the primary modality for hypertrophy and strength. No. But is could it be a form of resistance training. You are moving against body weight.
Jonathan Fields (00:58:14) – Yeah. I mean that makes a lot of sense to me. I actually owned a yoga center in New York in the early 2000 and taught for seven years. And a couple years into that, I actually ended up co investigating again.
Jonathan Fields (00:58:26) – My name was nowhere on this, but with a human performance lab at a local university. We brought a whole bunch of my students into a lab and hooked them up to all sorts of equipment we were more focused on. We had a standardized sequence of vinyasa yoga sequence, which is like very dynamic and very physical, and we were measuring the metabolic cost of it. So we didn’t measure more like the resistance effect. But the actual investigators in the lab were blown away at how fierce and potentially be. Again, like a beginner isn’t going to start with the type of sequence that we were doing in the lab. You know, it is the type of thing where even if you adapt and it becomes easier, it’s the type of pursuit where you can continue to adapt the activity itself. I want to ask you one other thing, though, about resistance training, about exercise in general, because so many people just hear the word and they’re just they roll their eyes. They have the worst possible association with it.
Jonathan Fields (00:59:25) – They want nothing to do. With it. We’re not even going to talk about Ms.. Like, well, I don’t want to bulk up and stuff like that, but just people’s experience so often with all forms of exercise, especially resistance training, is really negative. I have always believed that, yes, you need a sort of minimum viable dose. I know you talk about sort of like the minimum effective dose, but at the same time, do you have a take on whether it makes a difference to try and experiment with a bunch of different things, to try and find something that you are genuinely drawn to that is genuinely in some way, shape or form, joyful for you?
Dr. Gabrielle Lyon (01:00:01) – You do. And also there is this barrier. Things that we’ve never done are uncomfortable, and the only way that you build confidence to do something is to actually do the thing. When you go to the gym, you’ll see most of the women are on the cardio vascular activity equipment, and most of the guys are in the weight room, and a lot of women will tell themselves, so I just don’t like to do it.
Dr. Gabrielle Lyon (01:00:26) – And many of them haven’t tried. And you are always going to feel uncomfortable and you might feel self-conscious and you still have to do it anyway. And what you will find is you will likely find that you fall in love with the concept and the kind of goal of being strong, and there’s a million different ways to do it. The only way that you’re going to cultivate capacity is to be able to move past any mental discomfort about it. But yes, you should find something that you love. And I say that with a little bit of a warning in that you must examine the way that you’re thinking about the activities now.
Jonathan Fields (01:01:06) – And as somebody who before I was actually in the yoga world that I was, I actually owned a fitness facility. That’s so cool. So I like I saw the culture and our goal was basically we looked at the defining elements of the culture of your traditional big box facility, and we basically made a list and said, what is the opposite of all of this? Because so much of what you’re talking about is, you know, there is so much gender stereotyping within a facility that you might go into, and it’s not necessarily the the activity itself that we don’t like.
Jonathan Fields (01:01:40) – It’s all of the culture and it’s everything that’s wrapped around it that makes us feel really uncomfortable. And if we can either find a place where that gets stripped away and there are more and more of those, I think there are these days, or just tell ourselves, like, I don’t have to buy into this. And just like, let me focus on the thing. How does it feel? Your inside, I think was really important to it’s going to feel uncomfortable in the beginning no matter what, because we got to learn a new thing. We got to learn new movements. We have to build the strength and the the ability to do it in a way that we feel competent. But once we get past that threshold, oftentimes things do feel really great, and we do look forward to it and really look forward to the way that it makes us feel after we’ve done it, too. And I think that’s something that’s important as well.
Dr. Gabrielle Lyon (01:02:27) – I agree, and you’ll never hear someone say, wow, I really regret doing that thing.
Dr. Gabrielle Lyon (01:02:32) – Even yoga. How many times have I had to drag myself to a yoga class? I never regret doing it. I always feel better after that 100%.
Jonathan Fields (01:02:41) – This is so interesting. The notion that, you know, maybe what if was in the lens out and start to focus less on okay, body fat is the main source of all of all that ails us and say, like being under muscled is a huge issue and and how it affects our health or well-being or metabolism, our risk for disease and then fold in, okay, so what do we do about this? How do we reimagine nutrition? How do we reimagine movement just so powerful? And I think at the end of the day, and this is a lot of what you write about, both directly, and I think sort of implied in a lot of this is there’s a sense of agency that comes with all of this, that often when we’re focusing on the body fat side of things, we don’t feel and I think that from a psychology standpoint, that’s really important.
Dr. Gabrielle Lyon (01:03:32) – That is beautifully said. And I really know that we together can shift this narrative. I know that we can do it. And I’m just so grateful that you’re giving me the platform to be able to share about this. So thank you.
Jonathan Fields (01:03:47) – Pleasure. So coming full circle, as we always do here, wrap with the same question in this container of Good Life project. If I offer up the phrase to live a good life, what comes up?
Dr. Gabrielle Lyon (01:03:59) – Well, the first thing for me is family, right? You’re close. Connection. I’m a mom of two little kids, and seeing them happy and healthy is is living a good life. And that means active, moving and healthy. And knowing that they can interface with this world in a way that is meaningful. And I also know that a stress free life will likely not be one filled with meaning.
Jonathan Fields (01:04:27) – Thank you. Hey, before you leave, if you love this episode, say that you’ll also love the conversation we had with David Sinclair about increasing lifespan.
Jonathan Fields (01:04:36) – You’ll find a link to David’s episode in the show notes. And of course, if you haven’t already done so, please go ahead and follow Good Life Project in your favorite listening app. And if you found this conversation interesting or inspiring or valuable, and chances are you did. Since you’re still listening here, would you do me a personal favor, a seven second favor, and share it? Maybe on social or by text or by email? Even just with one person? Just copy the link from the app you’re using and tell those you know, those you love, those you want to help navigate this thing called life a little better so we can all do it better together with more ease and more joy. Tell them to listen, then even invite them to talk about what you’ve both discovered. Because when podcasts become conversations and conversations become action, that’s how we all come alive together. Until next time. I’m Jonathan Fields signing off for Good Life Project.